There are actually 7 different types of weight loss surgery but my focus will always be on the sleeve and bypass. So let’s begin….
The most important takeaways when evaluating gastric sleeve vs bypass include:
- How they work: Both make you feel full sooner while eating. Only sleeve makes you feel less hungry generally, and only bypass reduces the amount of minerals your body absorbs.
- Qualify: Same requirements (30+ BMI with health problems, 40+ without)
- Hospital & recovery: Sleeve is a less complicated procedure with a shorter operating time. In-hospital and post-op recovery is similar.
- Weight loss & health improvement: Similar at 2 years post-op, but bypass patients tend to keep more weight off over the long-term.
- Insurance: Same (if your policy covers bariatric surgery, both sleeve and bypass will be covered).
- Cost: Same with insurance, bypass is about 25% more expensive without insurance.
- Diet & life after: Similar diet and exercise regimen, but bypass requires stricter supplementation and vitamin level monitoring.
- Complications & side effects: Both have a 99.8% survival rate. Bypass has a higher risk of complications and side effects.
|
The best weight loss surgery options for you depend on:
|
The Gastric Sleeve
Why Gastric Sleeve Works
- Reduced stomach size makes the patient feel full sooner after eating
- Removed portion of the stomach means fewer hunger-causing hormones are secreted, causing patient to feel less hungry generally
How Gastric Sleeve Is Performed
Gastric sleeve surgery, also called the Vertical Sleeve Gastrectomy (VSG), is
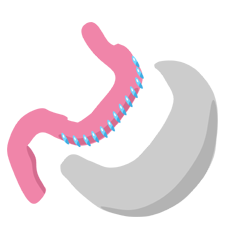
performed by removing a large portion of the stomach to create a long pouch that connects the esophagus to the small intestine. The pouch is stapled and the rest of the stomach is removed. Some surgeons take an additional step to reinforce the staple line, although whether that is effective is up for debate.
Studies evaluating gastric bypass vs. gastric sleeve have found very similar health improvement for diabetes, hypertension, sleep apnea, and most other obesity-related health problems, depending on which study is referenced.
The minimum gastric sleeve qualifications include:
- A body mass index (BMI) of 40 or more, OR
- A BMI between 30 and 39.9 with a serious obesity-related health problem like diabetes, high blood pressure, sleep apnea, high cholesterol, joint problems, and many others
However, protocols are a bit more stringent if you want insurance to pay, such as requiring a 35+ BMI and a completed medically supervised weight loss program.
Patients who qualify for gastric sleeve surgery usually:
- Are at least 80 lbs (36 kg) overweight
- Are between 18 and 75 years old
- Have a history of failed weight loss attempts (e.g., failed diets)
- Thoroughly understand that the procedure is just a tool; long-term success requires significant diet and lifestyle changes
The Gastric Bypass
Why Gastric Bypass Works
- Reduced stomach size makes the patient feel full sooner after eating
- Rearranged intestines causes the body to absorb fewer minerals
- Dumping syndrome symptoms deter patients from eating unhealthy foods
How Gastric Bypass Is Performed 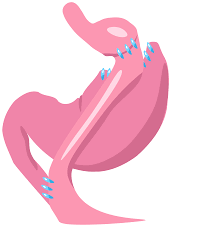
Gastric bypass, also called Roux-en-Y gastric bypass or RNY for short, is performed using the following steps:
- Cut and staple the top portion of the stomach to create a small pouch at the end of the esophagus
- Leave the remainder of the stomach attached to the top of the small intestines
- Go further down the small intestine, cut it, and attach it to the pouch
- Take the end of the small intestine that is still connected with the non-pouch portion of the stomach and attach it to the bottom of the “Roux limb.” This allows the digestive juices produced by the stomach to “meet up” with the food in the intestines.
The minimum gastric bypass qualifications include:
- A body mass index (BMI) of 40 or more, OR
- A BMI between 30 and 39.9 with a serious obesity-related health problem like diabetes, high blood pressure, sleep apnea, high cholesterol, joint problems, and many others
However, protocols are a bit more stringent if you want insurance to pay, such as requiring a 35+ BMI and a completed medically supervised weight loss program.
Patients who qualify for gastric sleeve surgery usually:
- Are at least 80 lbs (36 kg) overweight
- Are between 18 and 75 years old
- Have a history of failed weight loss attempts (e.g., failed diets)
- Thoroughly understand that the procedure is just a tool; long-term success requires significant diet and lifestyle changes
The chart below compares study results by condition for each procedure:
| Co-morbidity | Gastric Sleeve % Improved /Resolved | Bypass % Improved /Resolved |
| Dyslipidemia hypercholesterolemia | 64% | 63% |
| Diabetes | 55% | 83% |
| Hyperlipidemia (high levels of fat in the blood, high cholesterol) | 35% | 73% |
| High Blood Pressure (hypertension) | 68% | 69% |
| Joint/Bone Disease (osteoarthropathy) | 46% | 43% |
| Depression | most | most |
| Migraines | 40% | 57% |
| Pseudotumor cerebri | n/a | 96% |
| Venous Stasis Disease | 95% | 95% |
| Gastroesophageal Reflux Disease (GERD) | 50% | 80% |
| Non-Alcoholic Fatty Liver Disease | n/a | 90% |
| Mortality Reduction/ Life Expectancy (5 year mortality) | 89% | 89% |
| Metabolic Syndrome | 62% | 80% |
| Polycystic Ovarian Syndrome | most | most |
| Asthma | 90% | 80% |
| Obstructive Sleep Apnea | 62% | 98% |
| Stress Urinary Incontinence | 90% | 88% |
| Cardiovascular Disease | 100% | 79% |